A cancer diagnosis can often bring alarm and trepidation to patients and their families, and prostate cancer is no different. Following diagnosis, it is critical for patients to properly plan for prostate cancer treatment, understand the treatment process, and inform themselves as much as possible to minimize any unfounded worries and fears.
“Many patients come in, and they have a lot of anxiety,” says Steven G. Lester, M.D., F.A.C.R.O., a board-certified radiation oncologist, at Central Florida Cancer Care Center. “However, all that anxiety isn’t really necessary with prostate cancer.”
Upon visiting their radiation oncologist for the first time, many patients are surprised to learn that there is an extensive preparation process involved with prostate cancer, and they won’t be starting their radiation treatment as soon as they thought. “Most patients want to get started right away, and they get a little disappointed when I say that won’t be the case,” Dr. Lester continues. “The reason for that is that we have a lot of technology and planning that goes into treating prostate cancer.”
Preparing for Treatment
Initial preparation for image guidance radiation treatment for prostate cancer can take up to two weeks. Treating the prostate is more complicated because the organ cannot be detected on an X-ray machine.
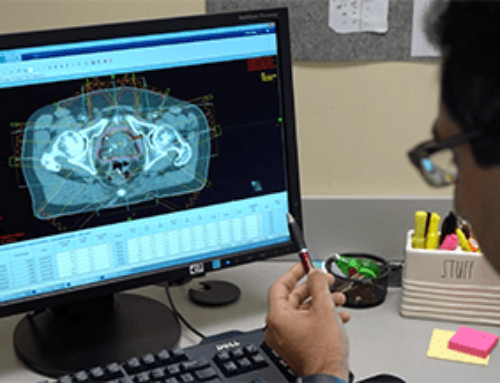
“For us to do image guidance, we place three little metal markers in your prostate to see (on X-ray imaging) where your prostate is on a daily basis,” says Dr. Lester. “Once the markers are placed, we complete a CAT scan and often an MRI to fuse the images so we can see exactly where your prostate is. We then undergo a planning process with the treatment planning computer which customizes the treatment to your anatomy.”
Once the plan is approved, a phantom treatment is performed on the treatment machine to ensure the computer determined all the correct calculations. “We bring you back and film you on the machine to make sure it lines up,” says Dr. Lester. “It takes a good seven to fourteen days to complete all the processes needed to make sure your treatment is accurate, precise and customized for you. That’s what goes on behind the scenes with your planning and treatment, and that’s why it takes about two weeks to get started.”
Types of Radiation for Prostate Cancer
There are two forms of radiation treatment typically used for prostate cancer, radioactive seed implant and daily radiation treatment utilizing image-guided radiation therapy (IGRT) or intensity-modulated radiation therapy (IMRT) techniques. Many patients are candidates for both or a combination of the two treatments.
“Radioactive seeds is an excellent technique when the patient has a small gland, a small localized cancer, and they can urinate well,” says Dr. Lester. “Patients who don’t urinate well because they have an enlarged gland, often get too much swelling from having 30 or 40 needles placed in their prostate. The advantage of that procedure is that it’s a one hour procedure.
”Radioactive seed treatment is performed in the operating room. Working in conjunction with a urologist, between 50 and 120 radioactive pellets (similar in size to the short side of a staple) are placed into the prostate utilizing needle sticks. Ultrasound in the rectum guides the placement of the seeds.
Most prostate cancer patients in the U.S. are treated with daily radiation treatments; they take place Monday through Friday, and take about fifteen minutes a day, with the beam time around three or four minutes. Patients experience no pain as if they were having a CAT scan or an MRI.
“The important thing to know is that there’s no sickness, no nausea, and no pain. The main hassle is coming in and out for treatment for nine weeks. While some patients may consider that a hassle, nine weeks of daily treatment to get rid of a serious disease is not so bad.”
IGRT: Modern Advances in Treatment
Before image-guided radiation therapy (IGRT), radiation oncologists needed to focurs radiation at a much larger perimeter around the tumor to ensure proper treatment. “Before the technology improved, we had to take about a two centimeter (roughly one inch) margin around the prostate to make sure we didn’t miss it,” says Dr. Lester. “The prostates move all day. They don’t move much, but they do move because if your rectum is distended with stool or gas, it is going to push the prostate in one direction. If the rectum is empty, the prostate will drop in the other direction.”
The advent of IGRT enabled cancer care physicians to visualize where the prostate would lie on a daily basis and spare significant amounts of healthy tissue from having to be exposed to radiation. “Once we developed image-guided radiation, we have been able to decrease the margins from two centimeters to 0.5 centimeters,” says Dr. Lester. “We treat a lot less healthy tissue and hit the target more effectively. IGRT has allowed us to put in a higher dose of radiation, resulting in longer, better term, local control, which hopefully will translate to cures.”
As part of their treatment preparation, patients can expect to spend ample time each day with the oncology staff filming, aiming, and watching treatment come and go from five to nine different directions. The process is designed to sculpt the dose of radiation and target it precisely on the prostate, treating less bladder, less rectum, less hip and giving patients a better cure rate with fewer side effects.
“There is a lot of technology involved with prostate radiation, and it takes time to get started,” says Dr. Lester. “It’s important you work with your doctor and his entire team to make sure your treatment is done properly. It’s critically important to reduce the side effects and improve the cure rate.”